What is allergy?

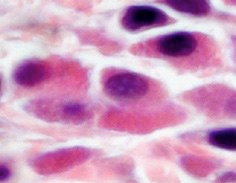
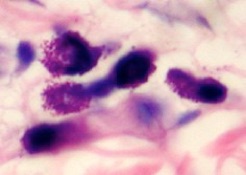
Mast cells in close up
Revised 4 April 2020
IMPORTANT The information provided is of a general nature and should not be used as a substitute for professional advice. If you think you may suffer from an allergic or other disease that requires attention, you should discuss it with your family doctor. The content of the information articles and all illustrations on this website remains the intellectual property of Dr Raymond Mullins and cannot be reproduced without written permission.
What causes allergy symptoms?
Underneath the lining of the skin, gut, lungs, nose and eyes are mast cells. These are designed to kill worms and parasites. Mast cells are like "land-mines", and contain "bags" filled with irritant chemicals including histamine. When these are released in small amounts, they cause irritation. In larger amounts, they can cause rashes, the sneezing of hay fever and the wheeze of asthma.
What happens during an allergic reaction?
Mast cells are armed with proteins called IgE antibodies, which act as remote sensors in the local environment. A person allergic to peanut, for example, will have IgE antibodies capable of recognising the shape of peanut protein (the allergen), in much the same way that a lock "recognises" the shape of a key. When this happens, mast cells dump their contents into the tissues, causing an allergic reaction. Depending on where the reaction occurs, it may result in itchy skin rashes, itchy watery eyes, sneezing and runny nose, cough and wheeze or even more serious symptoms known as anaphylaxis.
Common allergy triggers
We can have allergic reactions to what we swallow (food or medicines), what we breathe in / inhale (eg. dust mite, pollens, mold spores or animal allergen), what we touch (eg. plants, animals, perfumes, cosmetic preservatives) or what is injected (eg. insect stings, medications, blood transfusions).
Allergies tend to run in families
Allergic people have a greater than average tendency to produce IgE antibodies to common environmental substances. This tendency is inherited and occurs in around 2 in 5 people. If you have one allergic parent, for example, there is around a 1 in 3 chance of developing allergies yourself. If you have two allergic parents, the risk doubles. In other words, you can pick your friends but not your parents!
Allergy is increasing
Allergy is more common now than in our parents' and grandparents' generation. A number of careful studies in Australia and abroad have shown that the frequency of hay fever, asthma, eczema and even food allergy appears to have doubled in the last 30 years. It is a true increase, and not just because doctors are better at diagnosing allergies. In the last 10 years, similar increases in food allergy have also been observed in Australia, the UK and USA, particularly in peanut allergy. The explanation for this increase also remains unexplained, but eczema and delayed introduction of common allergenic food in early childhood increases the risk of food allergy in early childhood. Regular topical exposure of food to the skin (eg. food preparation workers or those using goats milk soap) increases the risk of food allergy in adults.
Why is allergy increasing?
There are many theories to explain the fact that the incidence of allergy has approximately doubled in the last 20-30 years in almost every country in which it has been studied. Theories include:
-Less exposure to parasitic disease in the developed world. This leaves one arm of the immune system with nothing to do except react against harmless "allergens".
-Lower rates of breast-feeding.
-Exposure to air pollution particularly exposure to particulate matter from diesel fumes. All of these increase the risk of asthma.
-Exposure to cigarette smoke in pregnancy increases the risk of asthma in offspring.
-The "hygiene hypothesis", whereby exposure to less infection early in life increases the risk of developing allergies.
-Low vitamin D levels, and many others
Unfortunately, there is no conclusive evidence at this time to easily explain the dramatic rise observed in recent generations
The Hygiene Hypothesis
Babies are born with an immune system which is inherently biased towards developing allergic-like reactions. These are called "type 2 response". A more balanced immune response is thought to require early exposure to infections. The first year of life appears to be the critical time in which this balance changes to a form of immunity that makes allergy less likely. Early exposure to infection is thought to "reset the balance" of the immune system by stimulating so-called "type 1 immune responses" instead. For example, allergic respiratory disease is less common in those growing up on farms with very close contact to farm animals. Recent studies have shown that multiple upper respiratory tract infections ("colds and flu's") in the first year of life may reduce the risk of developing asthma and hay fever by up to 50 %. There is also evidence that exposure to some gut bacteria may also play a role in modifying how the immune system develops in the first year of life, leading to trials of so-called “probiotics” in an attempt to reduce the risk, although results have been disappointing.
There is no convincing evidence that...
... food additives, preservatives, pesticides or vaccination contributes to a higher risk of allergy.
References
Ball TM et al. Siblings, day-care attendance, and the risk of asthma and wheezing during childhood. New Eng J Med 2000; 343: 538-43.
Sporik R et al. Exposure to house dust mite and the development of asthma in childhood. New England Journal of Medicine 1990; 323: 502-7.
Von Mutius E. The environmental predictors of allergic disease. J Allergy Clin Immunol 2000; 105: 9-19.
Matricardi PM et al. Exposure to foodborne and orofecal microbes versus airborne viruses in relation to atopy and allergic asthma: epidemiological study. BMJ 2000; 320: 412-7.
Wickens K et al. Antibiotic use in early childhood and the development of asthma. Clin Exp Allergy 1999; 29: 766-71.
Kramer U et al. Age of entry to day nursery and allergy in later childhood. The Lancet 1999; 353: 450-4.
Strannegard O et al. The cause of the increasing prevalence of allergy: is atopy a microbial deprivation disorder? Allergy 2001; 56: 91-102.
Mallol J et al. ISAAC findings in children aged 13-14 years an overview. ACI International 1999; 11: 176-82.
Holgate ST. Allergic disorders. BMJ 2000; 320: 231-4.
Salvi S. Pollution and allergic airways disease. Current Opinion in Allergy and Clinical Immunology 2001; 1: 35-42.