Tick allergy

IMPORTANT The information provided is of a general nature and should not be used as a substitute for professional advice. If you think you may suffer from an allergic or other disease that requires attention, you should discuss it with your family doctor. The content of the information articles and all illustrations on this website remains the intellectual property of Dr Raymond Mullins and cannot be reproduced without written permission.
Summary
Problems associated with tick bites include tick paralysis, transmission of infectious disease and occasionally, allergic reactions.
Introduction
Like other arachnids (such as spiders, scorpions and house dust mites), ticks have eight legs. They pass through a number of life stages from egg, to larva, nymph and then finally, the adult.
Health problems associated with tick bites include
•Transmission of infection
•Tick paralysis
•Allergic reactions to tick bites; and at times,
•Allergic reactions to red meat and gelatin.
The focus of this article is on allergic reactions to tick bites, and related allergic syndromes
Adult ticks cause the majority of health problems
Adult ticks (present mainly on the east coast of Australia although it is likely that other areas are also infested) cause the majority of the health problems in humans. Nonetheless, all stages of ticks are capable of provoking allergic reactions.
Larvae are very small ~ 1mm in size and can be difficult to see, nymphs slightly larger at ~ 2mm diameter with adult ticks (before a blood feed) being ~ 4mm in size, and are larger after a feed.
Adult ticks attach themselves to the tips of grass blades and vegetation, and transfer themselves to passing animals or humans. When humans are infested, the tick usually crawls up inside clothing. Adult ticks attach themselves strongly to their host by biting through the skin, and generally lodge in the skin of the head or neck or scalp of their host. The most common reaction is local irritation and swelling. While the “tick season” is often considered to range from around February to August, stages of the tick are present all year round, so there is really no one time when the risk of exposure completely disappears.
Tick paralysis
Tick saliva can cause paralysis in animals and humans (children are more susceptible), usually after the tick is embedded for 3-5 days. Symptoms are due to injected toxic proteins / neurotoxins. Symptoms include blurred vision, weakness of the limbs, and problems with coordination or speech. Treatment centres on removal of the tick. There is no vaccine to prevent reactions in humans.
Ticks as a source of infectious disease
Ticks can transfer infection from animals to human hosts, such as scrub typhus and Queensland tick typhus (spotted fever). Information on these disorders is beyond the scope of this article, but useful information can be found by contacting:
•TAGS (Tick Alert Group Support Inc., PO Box 95 Mona Vale, NSW 1660 (http://www.lowchensaustralia.com/pests/paralysis-tick/tick-alert-group-support.htm
•The Tick-Borne Diseases Research Unit, Royal North Shore Hospital, Pacific Highway, St Leonards NSW 2065.
•University of Sydney, Medical Entomology: http://medent.usyd.edu.au/fact/ticks.htm
•Victorian Health Department: http://ideas.health.vic.gov.au/bluebook/rickettsial.asp
•NSW Health Department: http://www.health.nsw.gov.au/environment/Publications/tick_alert_brochure.pdf
Allergic reactions to ticks
•Minor local itching and swelling is common at the site of a tick bite. That does not represent allergy.
•Sometimes large local swelling and inflammation can arise at the site of a bite and last several days.
•Serious allergic reactions (such as anaphylaxis) have also been described, in response to a number of species of tick species world-wide, including the so-called Australian paralysis tick, Ixodes holocyclus.
Serious allergic reactions occur when ticks are disturbed
Whereas most advice is to remove the tick as soon as possible using a fine pair of forceps, doing so in those with TICK ALLERGY is NOT advised. Almost invariably the allergic reaction occurs when the tick is disturbed, typically after attempts to remove it or, for example, after inadvertently disturbing the tick by scratching, deliberate attempts at removal or application of irritant chemicals like methylated spirits or kerosene may cause the tick to inject more allergen-containing saliva. This has implications for what should be done when a tick is discovered. See below for specific advice in those with tick allergy.
Managing reactions to ticks
Regardless of the type of reactions experienced after tick bites, the principles of management are:
•Try to reduce the risk of accidental tick bites;
•What to do if you find a tick lodged in your skin (and how best to remove);
•How to manage allergic reactions to tick bites;
•How to confirm a diagnosis of possible tick allergy;
•The relationship between tick bites and allergic reactions to red meat and gelatin in some unlucky individuals.
•Unfortunately, there is currently no vaccine to “switch off” tick bite allergy.
Reducing the risk of tick bites
The following measures may reduce the risk of tick bite:
The house
•Install animal proof fencing to keep bandicoots out of the yard where they can drop ticks.
•Create a hostile environment for ticks. They do not like dry hot conditions, so remove overhanging shady foliage and leaf litter plus keep the lawns short.
•Apply residual insecticides to the yard. Consult a pest-exterminator & check the product kills ticks.
•Treat pets to prevent ticks. Unfortunately the topical and oral products used in pets have not been tried in humans.
The person
•Wear long-sleeved shirts and long trousers when walking in areas where ticks occur
•Tuck trouser legs into long socks
•Wear a “coolie” style hat
•Wear light clothes, which makes it easier to see ticks
•Brush clothing before coming inside to remove ticks. Then place clothes in a hot clothes dryer for 20 min to kill ticks.
•Undress and check for ticks daily, checking carefully in the neck and scalp
•An insect repellent may help, particularly ones containing DEET (such as RID, Tropical RID or Tropical Aerogard or Bushmans) or Picaridin (OFF!).
•Consider buying and wearing permethrin-treated clothing when gardening or bush walking; look online for information on purchasing permethrin and how to treat clothing.
•In those with recurrent dangerous allergic reactions to tick bites, relocating to a non-bush area where ticks are not endemic can be considered.
What to do if you find a tick lodged in your skin and you are NOT allergic
The best advice varies according to whether or not you have had serious allergic reactions to tick bites. If you have minor irritation/local swelling only, the aim is to remove the tick as soon as possible to reduce the risk of tick paralysis or tick borne infectious disease. Thus remove the tick as per common advice to use fine forceps or tweezers between the skin and the tick mouthpiece. http://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_ticks.asp
What to do if you find a tick lodged in your skin and you are known to be ALLERGIC to tick bites
Eg. rash all over, anaphylaxis with difficulty breathing or a drop in blood pressure)
•If you are allergic to ticks, you should carry emergency medication (eg. an adrenaline autoinjector such as EpiPen or Anapen) and a means of summoning medical assistance (such as mobile telephone).
•If you find a tick, do not forcibly remove the tick*.
•Do not try to kill the tick using insecticide or chemicals (such as oil, turpentine, Kerosene, methylated spirits)*. Attempts to remove the tick or using these products can irritate the tick, do not result in immediate death of the tick and increase the risk that more allergen containing saliva may be injected. Indeed, most allergic reactions to ticks occur when an attempt is made to remove or poison the tick, or when it is disturbed (such as scratching).
•The consensus of medical advice is that the tick is killed first by freezing using ether containing sprays commonly used to treat warts such as “Wart-Off” or a similar product called “Tick-Off”.
•Seek urgent medical attention in case additional treatment is required. If you have not already removed the tick, it can then be removed under medical supervision where facilities are available to treat an allergic reaction.
•Follow you anaphylaxis action plan including use of an adrenaline autoinjector (EpiPen) if potentially dangerous allergic symptoms occur.
Additional information on using ether sprays to kill ticks
These are highly flammable products, so it is wise to use it away from naked flames and to not smoke around the area of use. It is important to note that Rapid cooling of the skin and thus skin irritation may occur
Confirming a diagnosis of possible tick allergy
At this time, there is no reliable skin or blood allergy test to confirm a diagnosis of tick allergy. Australian researchers have identified that the allergens causing problems are proteins in tick saliva. Diagnosis is largely based on the history of the reaction but some allergy test results have been associated with exposure to tick bites and clinical symptoms. Researchers have identified that the following blood allergy tests (RAST, ImmunoCap) are positive in the majority of those with serious allergic reactions to tick bites, that testing may assist in confirming diagnosis and that these tests can be ordered by any doctor:
•Beef and other red meat
•Alpha-galactose, a sugar molecule present in non human red meat as well as the gut of ticks
•Tryptase (an enzyme that is increased in those with a condition called mastocytosis, which is associated with an increased risk of allergic reactions to a number of allergic triggers including insect stings and tick bites)
Tick Bites and Red Meat Allergy
Australian allergic diseases physicians have described an association between tick bites and the development of red meat allergy, of whom a subgroup will also be allergic to meat and bone-derived gelatin. These finding have been confirmed by researchers in the USA and in Europe. The target allergen associated with these allergic reactions appears to be a sugar molecule known as alpha-galactose, present in tick guts, some worms, non-human red meat (eg. beef, pork, lamb, kangaroo whale, guinea pig) as well as gelatin. The degree of the allergic immune response (IgE) to alpha-galactose goes up after tick bites and seems to drop after many years of no exposure to ticks.
Symptoms of red meat allergy
Symptoms of tick bite allergy may range from itchy rash/hives, through to abdominal pain, difficulty breathing and collapse. Symptoms often occur at night, when larger amounts of meat are more likely to be consumed, but may not occur every time red meat is eaten. The reasons behind this remain uncertain. The onset of symptoms may also be delayed 3-4 hours after consumption. Around one third will react to gelatin, which also contains alpha-galactose. Reactions to animal milks are relatively rare but have been described.
Confirming a diagnosis of possible red meat allergy
Researchers have identified that the following blood allergy tests (RAST, ImmunoCap) are positive in the majority of those with serious allergic reactions to red meat, and that testing may assist in confirming diagnosis:
•Beef and other red meat
•Alpha-galactose, a sugar molecule present in non human red meat as well as the gut of ticks
•Tryptase (an enzyme that is increased in those with a condition called mastocytosis, which is associated with an increased risk of allergic reactions to a number of allergic triggers including insect stings and tick bites)
•By contrast, blood allergy testing to gelatin is usually negative (even in patients who have had clear allergic reactions to gelatin orally or by injection)
Skin allergy testing to red meat and gelatin is highly variable, with often minor reactions on skin prick testing using commercial extracts of red meat or gelatin, although testing with real red meat may give more reliable results, as may other skin testing techniques.
Dietary advice in those with red meat allergy
Those with allergic reactions to red meat are best advised to avoid all mammalian meat (beef, lamb, pork, goat, sheep meat, horse meat, kangaroo, guinea pig, whale) as well as all forms of gelatin. Gelatin is present in some food products, occurs as a binding agent in some medications as well as in intravenous blood substituted known as gelatin colloid (eg. Haemaccel, Gelofusine). Those with allergy to red meat/gelatin are also advised to wear a Medicalert bracelet warning of potential allergy to gelatin colloid as well. Further advice on dietary avoidance strategies may be found on the TIARA website (http://www.tiara.org.au ).
I also recommend those with tick/red meat allergy wear a MedicAlert bracelet just in case they end up in hospital after and accident are are given intravenous fluids containing gelatin.
Additional Web links
Tick Induced Allergies Research and Awareness (TIARA)
References
Quercia O, Emiliani F, Foschi FG, Stefanini GF. Anaphylactic shock to Argas reflexus bite. Allerg Immunol (Paris). 2005 Feb;37(2):66-8.
Hilger C, Bessot JC, Hutt N, Grigioni F, De Blay F, Pauli G, Hentges F. IgE-mediated anaphylaxis caused by bites of the pigeon tick Argas reflexus: cloning and expression of the major allergen Arg r 1.
Rolla G, Nebiolo F, Marsico P, Guida G, Bigo P, Riva G, Zanotta S. Allergy to pigeon tick (Argas reflexus): demonstration of specific IgE-binding components. Int Arch Allergy Immunol. 2004 Dec;135(4):293-5. Epub 2004 Nov 24.
Acero S, Blanco R, Bartolome B. Anaphylaxis due to a tick bite. Allergy. 2003 Aug;58(8):824-5.
Brown AF, Hamilton DL. Tick bite anaphylaxis in Australia. J Accid Emerg Med. 1998 Mar;15(2):111-3.
Moneret-Vautrin DA, Beaudouin E, Kanny G, Guerin L, Roche JF. Anaphylactic shock caused by ticks (Ixodes ricinus) J Allergy Clin Immunol. 1998 Jan;101(1 Pt 1):144-5.
Beaudouin E, Kanny G, Guerin B, Guerin L, Plenat F, Moneret-Vautrin DA. Unusual manifestations of hypersensitivity after a tick bite: report of two cases. Ann Allergy Asthma Immunol. 1997 Jul;79(1):43-6.
Veraldi S, Scarabelli G, Grimalt R. Acute urticaria caused by pigeon ticks (Argas reflexus). Int J Dermatol. 1996 Jan;35(1):34-5.
Humphery-Smith I, Thong YH, Moorhouse D, Creevey C, Gauci M, Stone B. Reactions to argasid tick bites by island residents on the Great Barrier Reef. Med J Aust. 1991 Aug 5;155(3):181-6.
Van Wye JE, Hsu YP, Terr AI, Moss RB, Lane RS. Anaphylaxis from a tick bite. N Engl J Med. 1991 Mar 14;324(11):777-8.
Solley GO. Allergy to stinging and biting insects in Queensland. Med J Aust. 1990 Dec 3-17;153(11-12):650-4.
Gauci M, Loh RK, Stone BF, Thong YH. Evaluation of partially purified salivary gland allergens from the Australian paralysis tick Ixodes holocyclus in diagnosis of allergy by RIA and skin prick test. Ann Allergy. 1990 Mar; 64(3):297-9.
Gauci M, Loh RK, Stone BF, Thong YH. Allergic reactions to the Australian paralysis tick, Ixodes holocyclus: diagnostic evaluation by skin test and radioimmunoassay. Clin Exp Allergy. 1989 May;19(3):279-83.
Gauci M, Stone BF, Thong YH. Detection in allergic individuals of IgE specific for the Australian paralysis tick, Ixodes holocyclus. Int Arch Allergy Appl Immunol. 1988;85(2):190-3.
Pearce RL, Grove DI. Tick infestation in soldiers who were bivouacked in the Perth region. Med J Aust. 1987 Mar 2;146(5):238-40.
Van Nunen SA, O'Connor KS, Clarke LR, Boyle RX, Fernando SL. An association between tick bite reactions and red meat allergy in humans. Med J Aust. 2009 May 4;190(9):510-1.
Commins SP, James HR, Kelly LA, Pochan SL, Workman LJ, Perzanowski MS, Kocan KM, Fahy JV, Nganga LW, Ronmark E, Cooper PJ, Platts-Mills TA. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-α-1,3-galactose. J Allergy Clin Immunol. 2011 Mar 29.
Mullins RJ, James H, Platts-Mills TAE, Commins S. The relationship between red meat allergy and sensitization to gelatin and galactose-alpha-1,3-galactose. J Allergy Clin Immunol 2012 (in press).http://dx.doi.org/10.1016/j.jaci.2012.02.038
Last reviewed 5 June 2020
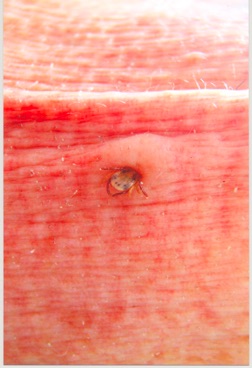
Tick buried into the skin of the neck