Latex allergy

IMPORTANT The information provided is of a general nature and should not be used as a substitute for professional advice. If you think you may suffer from an allergic or other disease that requires attention, you should discuss it with your family doctor. The content of the information articles and all illustrations on this website remains the intellectual property of Dr Raymond Mullins and cannot be reproduced without written permission.
Last reviewed 5 June 2020


Summary
Latex or rubber is a natural product obtained from the sap of the Havea tree. It is used in a number of medical and commercial products. Latex allergy is becoming a more frequent problem in health care workers and those who have had a number of operations.
What is latex?
Natural latex or rubber is a natural product obtained from the sap of the Havea tree. Preservatives, stabilisers and antioxidants may be added during manufacture to assist its stability. It may be dipped into a mould, then heated and dried. A dry powder lubricant (usually cornstarch) is often added to prevent the rubber surfaces from sticking together. Allergic reactions can occur to latex protein as well as the chemicals added to it, but not to cornstarch. Synthetic rubber can be made these days from petrochemicals. It is used in many commercial products such as latex paints and even the seals used in many asthma puffers! These products do not contain allergenic natural latex proteins and do not cause allergic reactions.
Latex has great physical properties
It stretches without breaking, can be molded into shape and provides a barrier to water and germs. That’s why it is so commonly used in commercial products. These include such things as rubber sheets, baby dummies, the nipples on the tops of baby bottles teats, rubber balls, balloons, washing-up gloves, condoms, diaphragms, rubber bands, clothing elastic, handles / grips as well as the stretch headbands that hairdressers use. For similar reasons, it has traditionally been used in many medical products and devices, although substitutes are now becoming more common. These include latex gloves, urinary catheters, tubing for barium enemas, rubber bungs in intravenous giving sets and sometimes drug vials, tourniquets used for taking blood, the rubber gum in self-adhesive bandages, dental drains and "rubber dams", some tapes, and anaesthetic tubing.
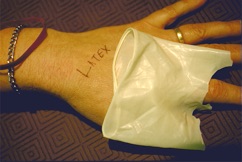
What Is A Latex Allergy?
A latex allergy is when a person has side effects from coming in to direct or indirect contact with rubber or latex containing products. There are 3 types of reactions:
Irritant dermatitis
This is not allergic. Irritation from washing with harsh soaps or sweating under gloves results in rough, dry and scaly rashes. Even though irritant dermatitis is not an allergy, absorption of latex through damaged skin increases the risk of later developing allergy with continued exposure.
Contact allergic dermatitis
This is a reaction to the chemicals added to rubber during manufacture, not due to an allergy to latex proteins. Rough and scaly and sometimes weeping rashes can develop within a few days of contact. As with irritant dermatitis, absorption of latex through damaged skin increases the risk of later developing allergy with continued exposure.
Immediate allergic reactions to latex protein
These allergic reactions are directed to the protein from the sap of the rubber tree. Contact with latex releases the irritant chemical “histamine” into the tissues. Reactions can occur within minutes and include hives or swollen lips or face at the site of contact. Others will develop irritation after wearing a condom, having a Pap smear taken or after dental treatment. Hay fever-like symptoms may occur, typically in hospital settings where frequent changing of gloves can result in suspension of fine latex particles in the air. More serious reactions can occur. In very sensitive patients, rapid absorption of latex through moist surfaces like as the mouth, nose, throat, vagina, rectum ("back passage") can result in difficulty breathing, a drop in blood pressure or even shock and anaphylaxis.
Who is at risk?
Most people who are allergic to latex have had frequent exposure to latex in the past. The vast majority are nurses, doctors, dentists, or patients who have had a number of operations, such as those with spina bifida. Many are also allergic to other substances such as grass pollens or dust mite proteins. In other words, they usually already have other allergic disease such as asthma, hay fever or eczema. Some unlucky individuals develop latex for no obvious reason.
Food allergy and latex
Proteins in latex are present in some foods as well. Latex-allergic people sometimes find that some foods cause an itchy mouth or throat swelling. The most common foods described are banana and avocado and sometimes kiwi fruit, passionfruit, plums, strawberry, tomato or other fruits. These foods do not have to be avoided routinely – only if they cause problems.
Testing for latex allergy
Your doctor will normally ask a series of questions that may help to identify the cause of your problem. This will often be followed by allergy testing to help confirm or exclude the presence of allergy. These include skin prick tests, blood allergy (RAST) tests or “patch tests” in those with a delayed contact allergic dermatitis.
Management of Latex Allergy
Avoid latex. Latex allergy can not be "turned off". The only treatment is careful avoidance. The more that you are exposed to latex, the more allergic you may become. It is therefore important to avoid latex as much as possible, even if your own latex allergy is relatively mild.
Wear a MedicAlert bracelet. If you are unconscious or confused and need emergency treatment, then the nurses and doctors will be aware of this and again will make alternative arrangements for your treatment.
Choose your career carefully. You may wish to consider avoiding jobs where latex is difficult to avoid such as nursing, dentistry, medicine, veterinary science, hairdressing or food preparation.
Contraception. There are a number of barrier contraceptives available that are latex free. The female condom "Femidom" is latex free and available in the UK and Australia. See also www.condomcountry.com.au for relevant products or ask your pharmacist.
Tell your doctors and dentists!
If you are going to undergo any medical or dental treatment, it is important that you volunteer the fact that you are allergic to latex. This will allow time to ensure that non latex-containing gloves and devices are available. You must volunteer this information, even if you are not specifically asked. This is so that alternative preparations can be made to ensure that latex is not used. Telling the anaesthetist about your allergy 5 minutes before the operation is not good enough. You must tell your surgeon in advance as well.
What Other Precautions should you take?
Carry your own supply of non-latex gloves (such as vinyl or nitrilite: available from pharmacies). Don't rely on others to have them in an emergency. They MUST be used when you have procedures such as dental work, blood tests, pap. smears etc. If you are a health care worker, you will need special consideration at work to minimise ongoing exposure, such as the provision of non-latex gloves for yourself, and the use of non-powdered gloves for co-workers. The biggest risk for you will be exposure to airborne latex particles from powdered gloves. This will need to be discussed with your superiors.
If you are not latex allergic but your job involves frequent exposure to it…
Request that non-powdered latex gloves be supplied. This is because airborne latex particles increase the risk of developing latex allergy.
Look after your hands. Have irritation or rashes evaluated by a doctor. An intact skin barrier reduces the risk of developing latex allergy.