IgE

IMPORTANT The information provided is of a general nature and should not be used as a substitute for professional advice. If you think you may suffer from an allergic or other disease that requires attention, you should discuss it with your family doctor. The content of the information articles and all illustrations on this website remains the intellectual property of Dr Raymond Mullins and cannot be reproduced without written permission.
Summary
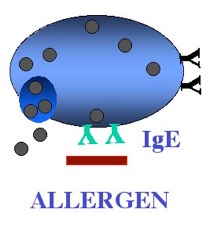
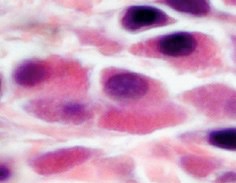
Underneath the lining of the skin, gut, lungs, nose and eyes are so-called mast cells. These are designed to kill worms and parasites. Mast cells are like “land-mines”or “bean-bags” filled with irritant chemicals including histamine. When these are released in small amounts, they cause local itch and irritation. Mast cells are armed with proteins called IgE antibodies, which act as remote sensors in the local environment. A person allergic to grass pollen protein, for example, will have IgE antibodies capable of recognising the shape of pollen protein (the allergen), in much the same way that a lock “recognises” the shape of a key. When this happens, mast cells are triggered to dump their contents (such as histamine) into the tissues, causing an allergic reaction within minutes. Release of histamine can trigger symptoms of hay fever, asthma and food allergy.
History
The history of allergy makes interesting reading. In the 1870's, grass pollens were identified as the trigger for seasonal hay fever symptoms in the U.K., based on using crude pollen extracts to trigger symptoms if placed into the eye, and the use of similar extracts for skin allergy testing. By 1916, skin testing was being used confirming the presence of allergy, although how it worked was not totally clear at the time.
In 1919, Ramirez described a patient who developed horse-allergic asthma for the first time after he had been transfused using blood from a horse allergic donor. This suggested that "allergy" could be transferred by a blood-derived factor. This theory was confirmed by Kustener (who was fish allergic) by injecting his own serum into a colleague's skin, thereby passively transferring sensitivity to fish with skin testing to his colleague.
It was only in 1967 that Ishizaka discovered Immunoglobulin E as this serum factor, named for the "Erythema" induced by skin testing. Five ywarsIgE receptors were identified on mast cells and basophils, and to show that cross-linking of surface IgE would lead to degranulation and mediator release.
IgE production
IgE is produced by plasma cells, predominantly in lymph tissue next to the respiratory and gastrointestinal tracts. Adult levels of IgE are reached by the age of 10 - 15 years, and are present in a non-linear distribution in the population. Seasonal variation two to four fold of IgE occurs throughout the year.
IgE in health and disease
It is often wrong assumed that a high IgE is the likely cause for obscure symptoms, and that a normal result virtually excludes the diagnosis. In fact, high IgE is observed in only 30% of patients with hay fever, 60% of patients with asthma and in 80 - 90% of patients with significant atopic eczema. An elevated IgE in conditions such as hives, for example, usually means that the patient has one of these other conditions, rather than a food allergy as a cause of their hives !
IgE may also be increased in 10 - 20% of patients with non-allergic rhinitis or non-allergic asthma, or in conditions like allergic bronchopulmonary aspergillosis, some forms of immunodeficiency, neoplasia such as lymphoma, and parasitic disease and even in otherwise healthy people without allergy.
Total IgE therefore has a poor track record for predicting whether allergy is a cause of symptoms which is why I rarely measure it. If an allergy test is needed, it is much more useful to measure the amount of specific IgE directed against specific triggers. eg. ryegrass, cat allergen or peanut.
It should be remembered, however, that not all patients with symptoms of asthma, respiratory disease or eczema are proven to be allergic. The implications are that allergen avoidance measures and immunotherapy are not warranted.
Last reviewed 29 May 2020